Pediatric Neurology & Neurosurgery

Life-Changing Neurology and Neurosurgery Care for Children
Meet Our Pediatric Neurology and Neurosurgery Specialists
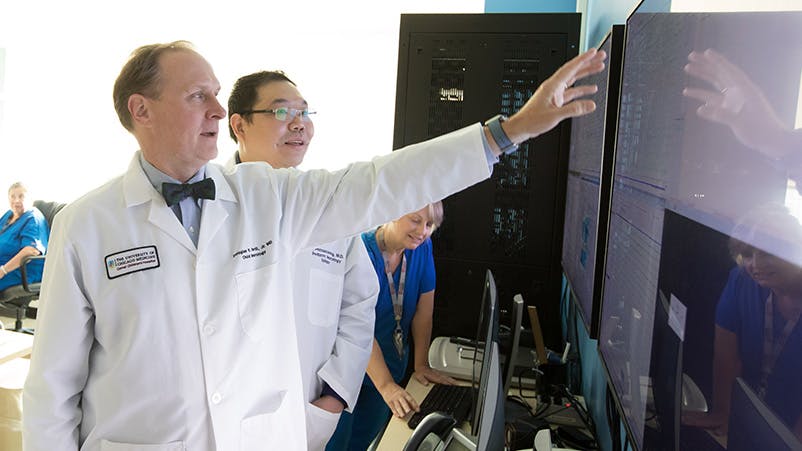
The experts on our team pride themselves on being at the forefront of pediatric care. That's why our comprehensive team of pediatric specialists, nurses and support staff spends so much one-on-one time with all of the children and their families, as we know first-hand the profound effect that caring and compassion can have on a child's prognosis.

Leaders in Pediatric Neuroscience
Our patients often have access to new treatments years before they are widely available at other medical centers. Many of our neurologists and neurosurgeons are actively exploring promising new therapies for neurocutaneous disorders, epilepsy, neurofibromatosis and other neurological problems that affect children.
Neurological Conditions in Children We Treat
Pediatric Neurology and Neurosurgery Locations in Chicago, South Suburbs and Northwest Indiana
Request a Pediatric Neurology or Neurosurgery Appointment
To speak to someone directly, please call 1-773-702-6169. If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
* Indicates required field